At-Home Treatment, Facilities Fees, and Consensus
There’s a tactic agreement that safety and efficacy are not going to be the barrier to rolling out psychedelic medicine— but rather, delivery will prove most challenging.
Who can deliver the treatment, in what environment, and who is going to pay for it?
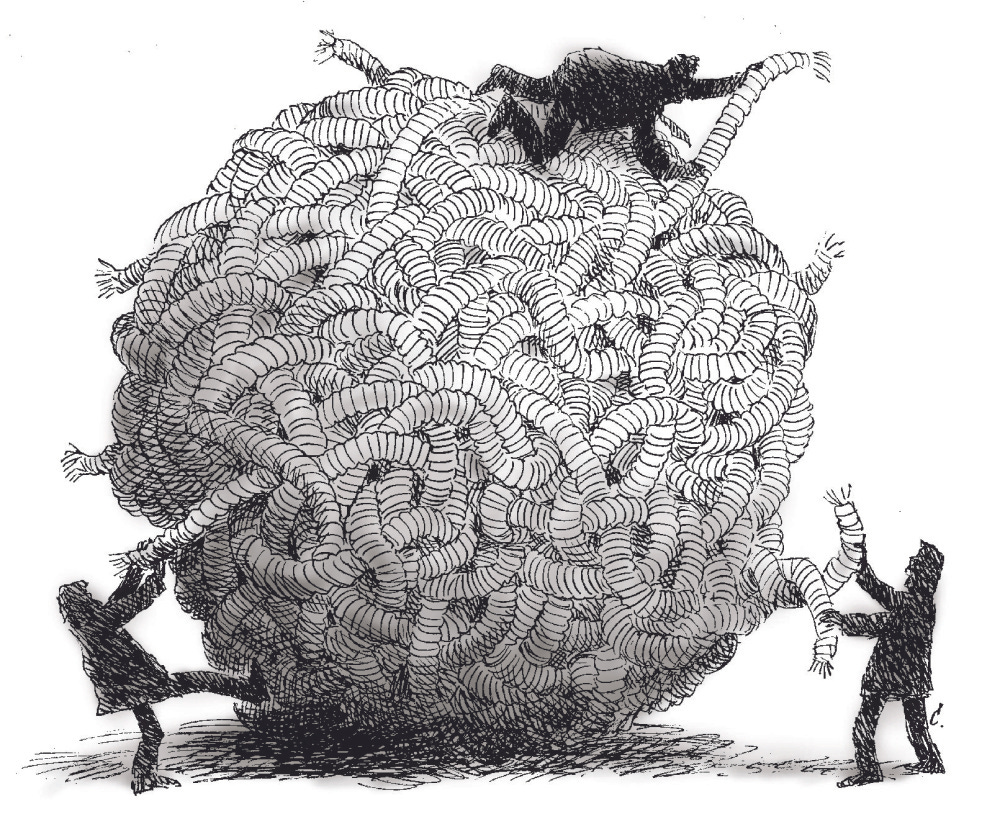
If drug development is sophisticated gambling, the building of the delivery infrastructure for psychedelic therapies is untethering a Gordian Knot.
In December, in “The 'Last Mile Problem' for Psychedelic Medicine,” we noted:
“The last mile could prove more challenging than the psychedelic community is anticipating because
The compounds in question are combined with psychotherapy and the therapists require additional training and credentialing
The clinics will need to meet certain criteria to be allowed to administer the treatment
Insurance and third party reimbursement is not a guaranteed
The patient population has a condition that makes life more challenging to get out of bed and make it to appointments and keep appointments
The cultural baggage the psychedelics carry
The built-in frenzied enthusiastic community of psychonauts…
For all of these reasons, the last mile will not be straightforward.”
Add to this list that healthcare is a modern hellscape in which stakeholders extract value while providers and patients are the last considerations.
The MAPS’ MDMA for PTSD protocol, barring extreme events, will be the first approved psychedelic therapy with corresponding Risk Evaluation and Mitigation Strategy (REMS), which will impact facility and credentialing costs, labor costs, and other cost adding measures. These, of course, make sense to have in place for the rollout of such a “new” and unique form of treatment. (Treatment entails a series of preparation sessions, three dosing sessions lasting 6-8 hours with two therapists present, and follow-up integration sessions. This protocol must be delivered in a clinical setting supervised by personnel with credentialing requirements that remain uncertain.)
This friction is a good thing in the early years and allows issues to arise while they might still be manageable.
However, the next iteration of psychedelic-assisted therapy research would do well to reduce some of these constraints. If the MAPS protocol is a starting place, and if the FDA is to loosen the reigns to allow for more flexibility, other study designs will need to be tested.
Scalability Three Ways
Unshackling the constraints of the first generation of psychedelic treatment will come about by modifying:
The molecule (shorter duration)—We can modify the duration, which several companies are working towards, perhaps most notably Bright Minds and Entheogenix.
The requirements on clinical infrastructure and provider credentials to make them more flexible—We can modify the personnel requirements. The suggestions here range from allowing 100% technology-enabled monitoring to group administration, thereby improving the patient-to-provider ratio.
Requirements for patient monitoring—And then we can modify the facility requirements.
In some of his presentations, Rick Doblin has a slide showing different varieties of a psychedelic clinic—one is on a mountain top, another in a strip mall—but the implication is that the dosing sessions will be delivered in a controlled environment as laid out in the REMS.
Delivering treatment at home or in small, independent practices is not often discussed in practical ways because of these precautionary constraints.
They also haven’t been evaluated enough yet, but we’re slowly seeing alternative models in research design.
A recent study evaluating psychedelic group therapy for HIV survivors showed hopeful results in patient outcomes and the feasibility of group therapy. Palliative care patients that have received Section 56 exemption in Canada are undergoing treatment at home. Advances in telehealth and recent regulatory leniency in light of COVID, a move towards “decentralized clinical trials” and remote monitoring all point towards the potential for safe administration, monitoring, and data collection at home.
I share the belief that psychedelic therapy can be safely and effectively directed at several indications. Academic and Investigator-initiated research should focus on evaluating different forms of delivery, including a patient’s homes and in small, independent practices. If proven safe and effective, these options would simplify the cost and complexity of treatment.
The restrictive REMS of early approved psychedelics, though necessary, will require administrative expertise in navigating the regulatory and industry landscape such that it will be difficult, if not impossible for an independent psychiatrist or small practice to administer these treatments.
As we covered last week, there are factions of stakeholders who have a “you’re either with us or against us mentality” around corporate involvement in psychedelics.
One area where consensus might be available between the “Daoists” and the “Confucianists” is limiting the exposure of psychedelic medicine to the more extractive areas of the modern healthcare system.
Enabling psychedelic treatments to be delivered by independent providers and a patient’s homes will reduce costs, stigma, and entanglement with the more extractive aspects of the healthcare system.
To accomplish this, research into at-home and more naturalistic settings must flourish.